The Centers for Disease Control and Prevention (CDC) has reported a concerning surge in cases of Candida auris, a drug-resistant fungus posing severe risks to those with compromised immune systems.
“The increases, especially in the most recent years, are really concerning to us,” said Dr. Meghan Lyman, chief medical officer in the CDC’s Mycotic Diseases Branch.
The Nightmare Scenario: A Warning from Experts

“It’s a potentially multi-drug resistant pathogen with the ability to spread very efficiently in healthcare settings,” warns Dr. Luis Ostrosky, a professor of infectious diseases at McGovern Medical School at UTHealth Houston.
His warning against ignoring the spread of such fungi paints a grim picture of a “nightmare scenario,” highlighting that these organisms represent uncharted territory for researchers.
Case Numbers Nearly Double

NBC News explains that a significant uptick in Candida auris infections has alarmed health officials, with cases nearly doubling in 2021, from 756 to 1,471, per data from the CDC.
The CDC has labeled the situation an “urgent antimicrobial resistance threat.”
Mississippi Grapples with Growing Outbreak

NBC News reports that in Mississippi, the health department faces a challenging outbreak of Candida auris, with at least 12 people infected and four “potentially associated deaths,” according to the state’s epidemiologist, Dr. Paul Byers.
He points out the prevalence of multi-drug resistant organisms like Candida auris among residents in long-term care facilities as a significant concern.
Fungal Threat Emerges in Washington State

NBC News reports that Washington state is grappling with its first known outbreak of Candida auris. Seattle and King County health officials have identified four individuals this month who tested positive for this potentially fatal fungus.
Despite its newfound presence in Washington, there have been no reported fatalities linked to the infection thus far.
Candida Auris Spreads

The escalation of Candida auris cases nationwide is alarming, with annual increases observed since 2016. NBC News reveals that health experts predict it’s a matter of time before this fungal infection appears across all states.
In Washington, the recent cluster signifies the state’s initial encounter with an infection that has been intensifying across the country.
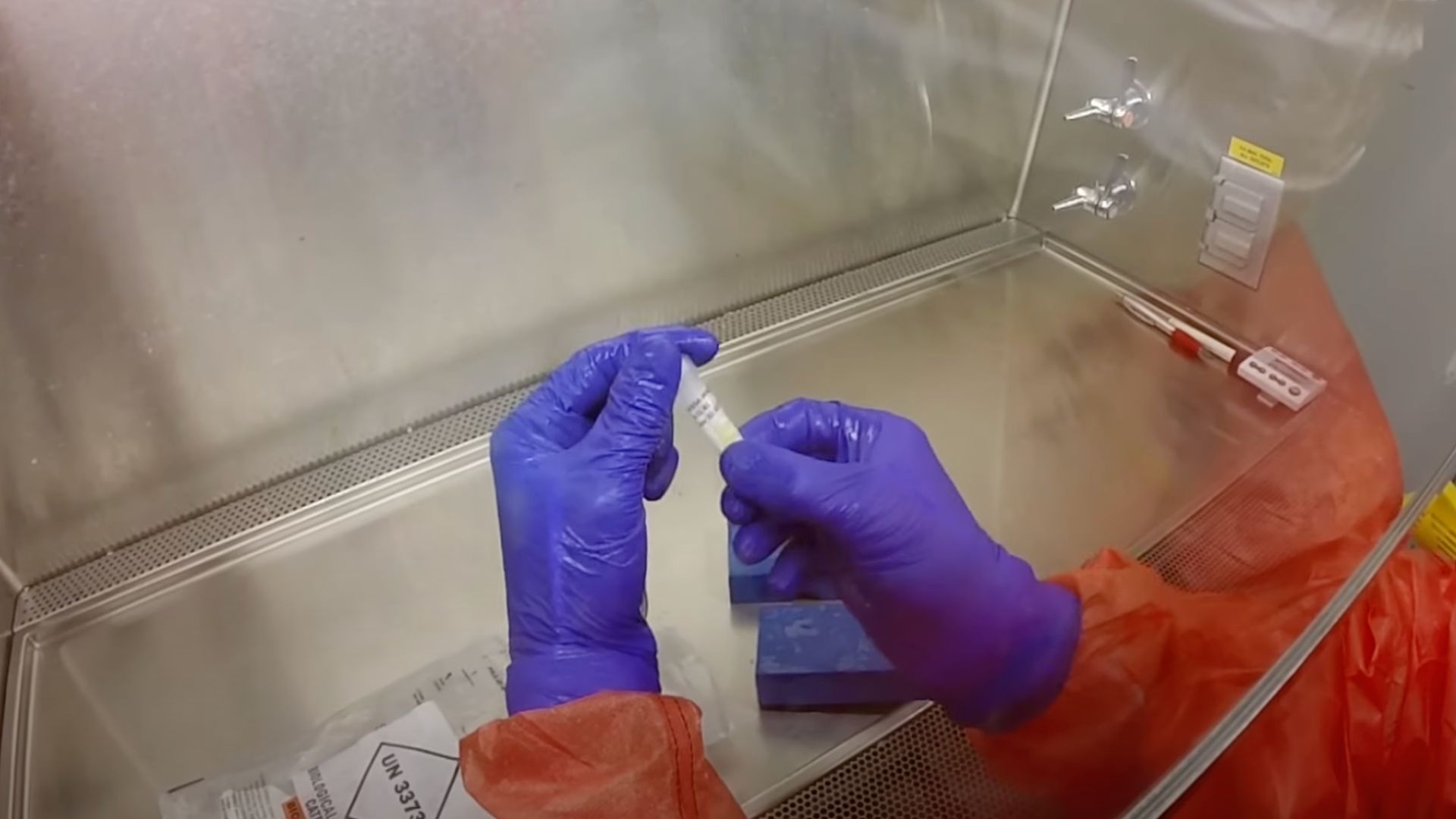
Detection at a Seattle Hospital

Three of the infected individuals were patients at Kindred Hospital Seattle First Hill, where the fungus was identified through a proactive screening program.
This program aims to detect infections early, ideally before patients show symptoms, showcasing the hospital’s commitment to preventing the spread of this dangerous pathogen.
Fourth Case Raises Broader Concerns

A fourth case emerged outside the initial hospital cluster, involving a patient in Snohomish County who had prior care at Kindred.
This case, reported by the public health department for Seattle and King County to NBC News, broadens the scope of concern, indicating the fungus’s potential to spread beyond initial outbreak sites.
Infection and Colonization Distinction

The health department clarified that one of the patients developed an actual infection, meaning the fungus penetrated body areas where it’s more likely to cause symptoms, such as the bloodstream or wounds.
The others were merely colonized, carrying the fungus without showing sickness. However, colonization still poses a risk as it can lead to infections or spread to others, highlighting the nuanced challenges in managing Candida auris.
Proactive Measures at Kindred Hospital

In response to the outbreak, NBC News reports that Kindred Hospital implemented strict isolation and enhanced cleaning protocols for the affected patients, who remain asymptomatic.
The hospital’s statement emphasized these measures aim to prevent the fungus’s spread, ensuring the safety of other patients and staff. This proactive approach is vital in containing such infections, demonstrating the hospital’s commitment to patient care and infection control.
A Global Concern

First identified in Japan in 2009, Candida auris has become a global health concern.
The CDC’s request in 2016 for U.S. labs to report cases brought to light the infection’s presence, with records tracing back to 2013. This historical context emphasizes the fungus’s rapid spread and the critical need for continued surveillance and research to combat this public health threat.
The Importance of Early Detection

The detection of Candida auris in Washington through routine screenings highlights the importance of early identification in managing infectious diseases.
By catching the fungus before it causes symptoms or spreads further, healthcare facilities can implement targeted interventions, potentially saving lives and preventing larger outbreaks.
Public Health Response and Awareness
The response to the Candida auris outbreak in Washington reflects a broader public health initiative to combat emerging infectious diseases.
Raising awareness, enhancing surveillance, and implementing effective control measures are key components of this response, aiming to protect communities and prevent future outbreaks. Public health departments play a critical role in coordinating these efforts, emphasizing the importance of preparedness and public education.
Combating Candida Auris

As Candida auris continues to pose a significant health challenge, the focus on research, prevention, and treatment strategies is more crucial than ever.
Understanding the fungus’s behavior, transmission, and resistance patterns will be key in developing effective countermeasures. The healthcare community and public health officials are at the forefront of this effort, working tirelessly to safeguard public health against this emerging fungal threat.
Widespread Detection and Treatment Resistance

The presence of Candida auris in more than half of U.S. states has raised alarms, particularly due to the fungus’s resistance to common treatments.
“We’ve seen increases not just in areas of ongoing transmission, but also in new areas,” Dr. Lyman remarked.
Rise in Asymptomatic Carriers Complicates Control Efforts

The CDC’s findings on the increase in asymptomatic carriers of Candida auris illustrate the complexity of controlling its spread.
The Mirror reports that individuals carrying the fungus without symptoms can inadvertently transmit it to more vulnerable populations.
Global Emergence of Candida auris Preceded Initial Discovery
Originally identified in 2009 , the history of Candida auris extends further back, as re-examined data revealed earlier instances of the fungus.
Dr. Graham Snyder, medical director of infection prevention at the University of Pittsburgh Medical Center, noted that this pattern is common with pathogens, which can start out extremely rare before becoming widespread.
Healthcare Facilities Struggle to Contain Spread

Containing Candida auris within healthcare facilities presents significant challenges, as the fungus can survive on various surfaces.
Dr. Waleed Javaid, an infectious disease expert, emphasized its extreme survivability to NBC News, necessitating rigorous cleaning protocols, including bleach and UV light, to prevent transmission to patients, especially in intensive care units.
Infection Risk Limited to Vulnerable Populations

The risk of Candida auris infection remains primarily with those who have weakened immune systems or use invasive medical devices.
“This is an infection that occurs in extremely ill individuals who are usually sick with a lot of other issues,” Dr. Javaid said, providing some reassurance to the general population about the risk of infection.
CDC Documents Steep Increase in Infections and Colonizations

From 2019 to 2021, the number of Candida auris infections rose dramatically, with a 59% increase followed by a 95% increase, respectively, NBC News reports.
The CDC also reported a significant rise in colonization rates, indicating a growing public health concern that requires immediate and comprehensive action.
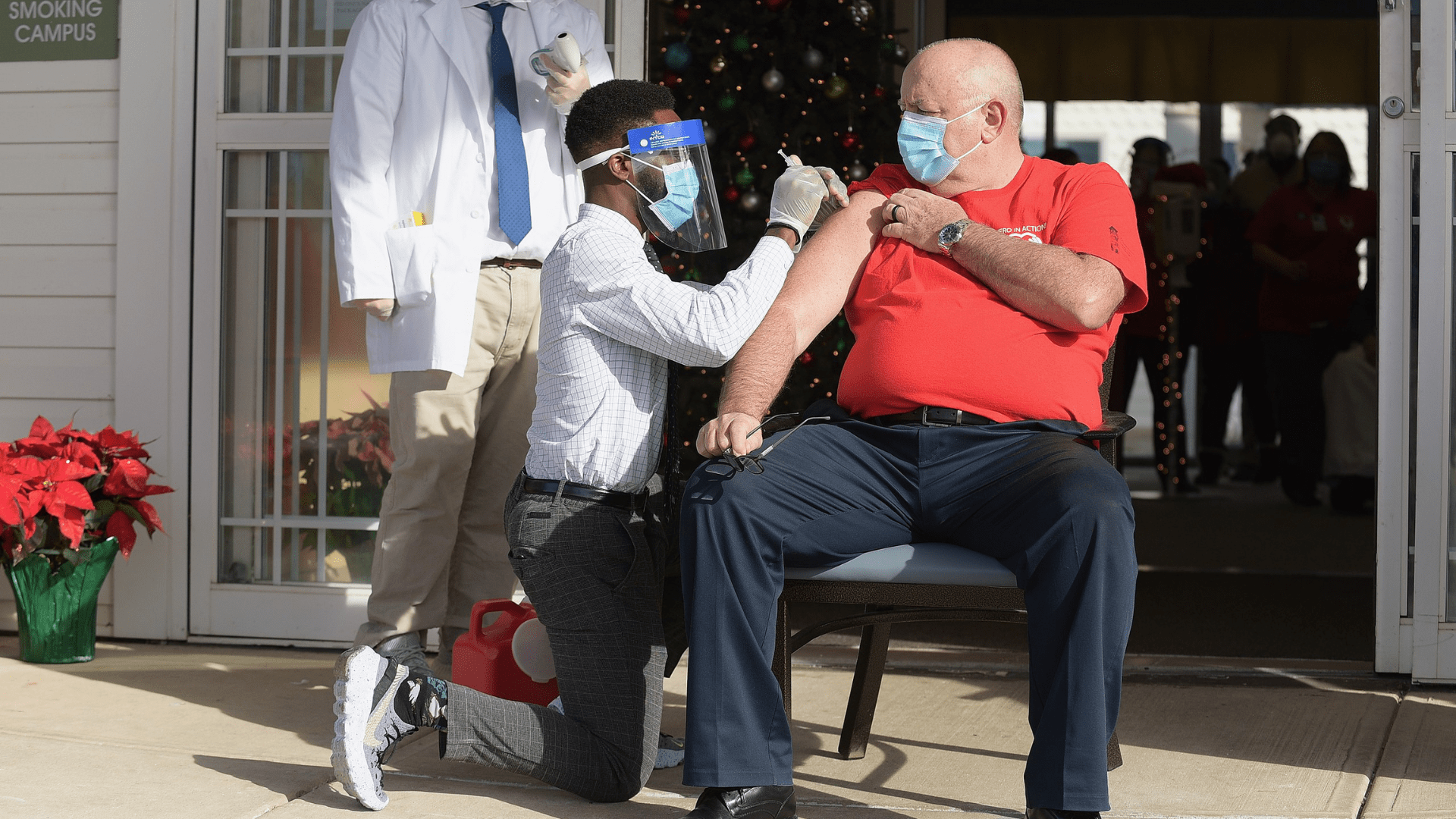
Urgent Call for Enhanced Infection Control Measures

In response to the escalating threat of Candida auris, the CDC emphasizes the need for improved surveillance, laboratory capacity, and adherence to infection prevention and control measures.
“The increases, especially in the most recent years, are really concerning to us,” Dr. Lyman reiterated, calling for urgent action to prevent further spread.
Recognition of Candida auris Threat

The inclusion of Candida auris on the World Health Organization’s list of “fungal priority pathogens” marks its recognition as a significant global health threat, BBC News notes.
This designation highlights the necessity for international collaboration to address the challenges posed by the fungus and to implement effective control strategies.
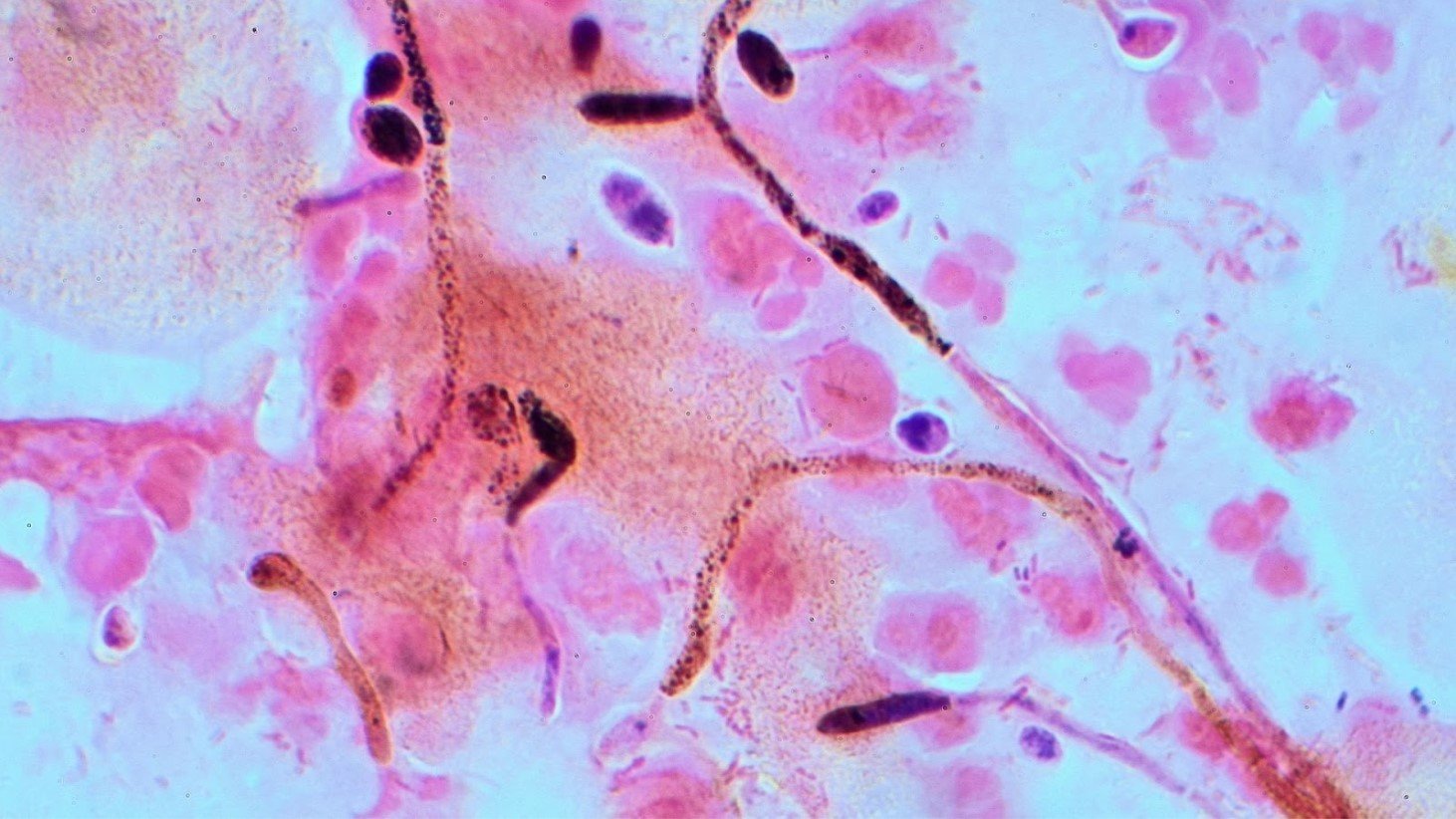
The Problem of Candida auris

Candida auris possesses the ability to infiltrate the bloodstream and disseminate throughout the body, often complicating treatment due to the pre-existing acute or chronic conditions of affected individuals.
Confronting this fungal infection is challenging as it frequently exhibits resistance to conventional antifungal medications, necessitating high doses of multiple drugs for effective clearance.
Candida auris Has Spread Globally

Transmission of Candida auris predominantly occurs within healthcare settings, particularly in hospitals, where contaminated surfaces like medical equipment and furniture serve as potential vectors.
Person-to-person transmission also contributes to its spread. Despite being identified in various global regions, including North and South America, East and South Asia, and southern Africa, distinct regional strains suggest independent development rather than cross-continental transmission.
R

Research suggests that Candida auris can survive on surfaces for weeks.
Notably, recent outbreaks of Candida auris have been documented in over 30 countries since its discovery in 2009, prompting the Centers for Disease Control and Prevention (CDC) to classify it as an “emerging pathogen.”
The Symptoms of Candida auris

The most common symptoms of a blood infection resulting from Candid auris are fever, chills, sweats and low blood pressure.
While fever and chills are common, they are non-specific and may overlap with symptoms of other infections. Complicating matters, individuals with Candida auris are often undergoing treatment for other conditions, making symptom identification challenging. The manifestation of symptoms is further influenced by underlying health conditions.
Who is Most At-Risk of Candida auris Infection?
The CDC notes that those most at risk from Candida auris are people with serious underlying medical conditions, requiring complex medical care.
Additional risk factors encompass diabetes, blood cancers like leukemia or lymphoma, immunocompromising conditions, prior exposure to multiple antibiotics, and the presence of medical devices like catheters, breathing tubes, and feeding tubes.
Understanding Candida auris Infection and Transmission Dynamics

The ability of Candida auris to spread in healthcare settings, especially among patients with prolonged hospital stays, adds to the urgency in addressing its rise.
By disseminating this knowledge, effective prevention measures can be implemented, contributing to the collective efforts to mitigate the impact of Candida auris on global health.








































