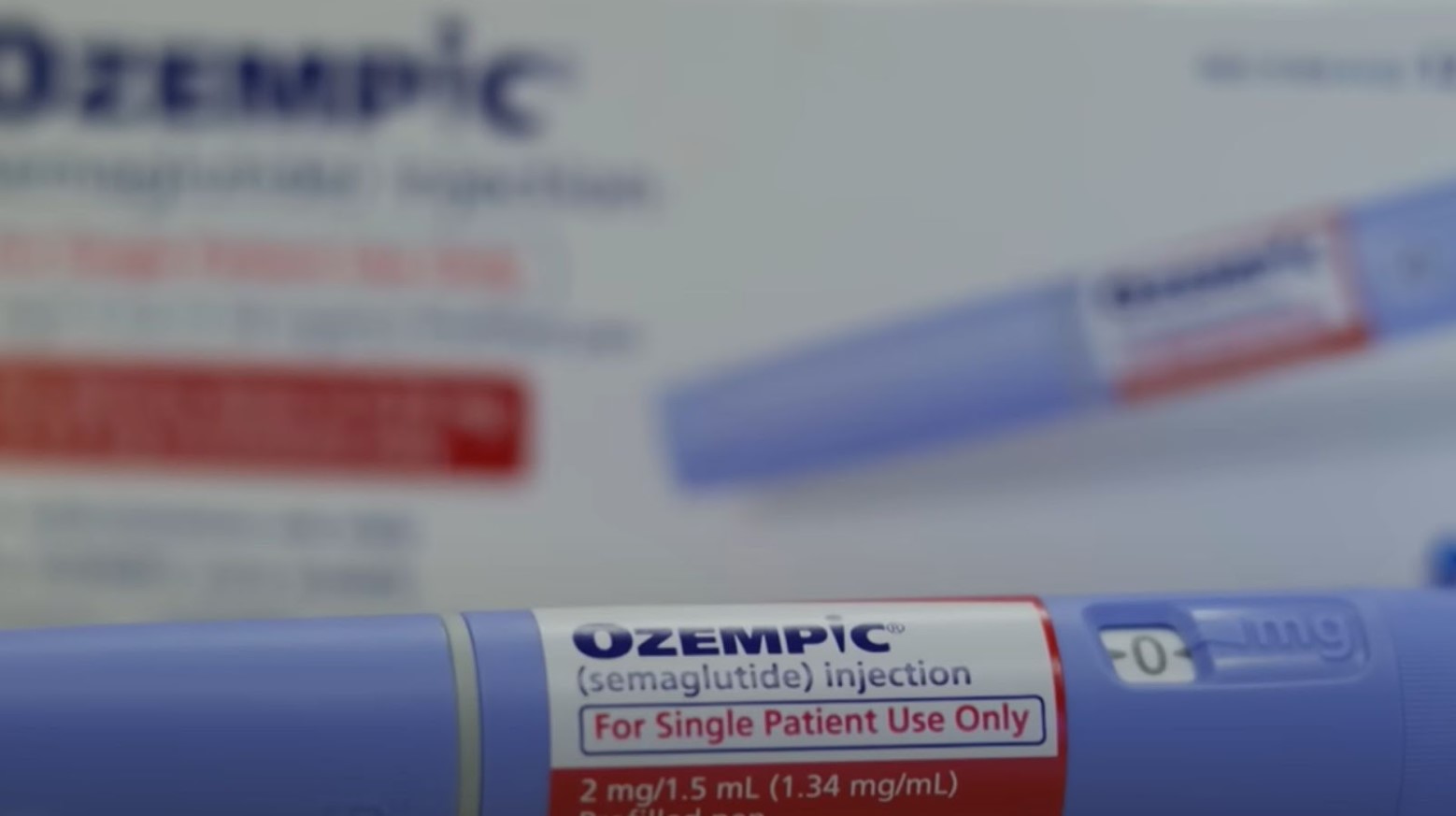
In an unprecedented move, children as young as 6 are being enrolled in a trial to test the effectiveness of weight loss injections, specifically semaglutide, known commercially as Ozempic and Wegovy. This bold step, sponsored by Danish pharmaceutical giant Novo Nordisk, marks a pivotal moment in the battle against child obesity in the U.K.
The decision to include children in such trials stems from a desperate need to address the increasing rates of obesity among young populations. Critics, however, express concerns over potential side effects and the long-term implications of administering such powerful drugs to children.
The Science Behind the Jab

Semaglutide operates on a simple yet profound principle: it tricks the brain into feeling fuller for longer periods by slowing digestion and reducing appetite (via the Mayo Clinic). While this mechanism is effective in adults, it raises questions about its application in younger, developing bodies.
The drug’s ability to influence weight through brain chemistry highlights its potential as a revolutionary tool in obesity treatment. However, this approach’s novelty brings with it an array of unknowns, especially concerning its effects on children’s overall health and development.
Weighing the Risks

While semaglutide has shown promise in adult weight loss, its side effects cannot be overlooked. According to Drugwatch, reports link the drug to a range of adverse effects, from nausea and digestive issues to more severe concerns like gallstones and increased suicidal thoughts.
For children, whose bodies and minds are still developing, the stakes are particularly high. The long-term health impacts of semaglutide on young users remain a mystery, resulting in the need for caution and thorough investigation within this trial.
Beyond the Injection

Integral to the trial is a requirement that child participants adhere to a diet and exercise regimen alongside their injections. This component is critical, as it acknowledges that medication alone is not a panacea for obesity (via The Daily Mail).
It also raises a pivotal question. If lifestyle changes are necessary for the drug’s success, could more emphasis on these changes render the need for medication obsolete? This aspect of the study highlights the multifaceted nature of obesity treatment, where medication, diet, and physical activity intersect.
The Global Study

This trial is not confined to a small cohort or a single location; it is a global effort involving more than 200 children across four NHS hospitals in Birmingham, Bristol, Leeds, and Liverpool.
The selection of participants is meticulous, focusing on those who are not just obese but also grappling with weight-related health issues like type 2 diabetes or high blood pressure (via The Daily Mail).
Voices of Concern

Critics of the trial argue that focusing on pharmaceutical interventions may divert attention from the root causes of obesity, such as poor diet and inadequate physical activity (via JAMA Network Open). They caution against seeking a “quick fix” through medication, advocating instead for more sustainable lifestyle modifications and preventive measures.
This criticism brings to light a broader societal challenge: addressing the environmental and behavioral factors contributing to the rise in childhood obesity.
A Celebrity-Endorsed Trend
The popularity of semaglutide among celebrities has skyrocketed, turning it into a highly sought-after weight loss solution. However, the experiences of public figures like Tracy Morgan, who gained weight while using Ozempic, serve as a reminder of the drug’s limitations (via E! Online).
These anecdotes highlight the importance of setting realistic expectations for semaglutide’s efficacy and recognizing that it is not a one-size-fits-all solution.
The Cost of Obesity

Obesity’s toll on the U.K.’s health system and the economy is staggering, with an estimated annual cost of £100 billion (via The Guardian). This figure encompasses medical expenses as well as the broader economic impacts, including lost productivity and increased care needs.
The financial burden of obesity underscores the urgent need for effective treatment strategies that can alleviate both the personal and societal costs of this growing health crisis.
Regulatory Hurdles

Despite semaglutide’s approval for use in overweight children aged 12 and above in the U.S. and EU, the U.K.’s National Health Service (NHS) awaits more conclusive evidence before making it widely available.
The current trial represents a crucial step in gathering the necessary data to potentially broaden semaglutide’s accessibility and application in treating child obesity within the NHS framework.
Looking Ahead
With the trial set to conclude in November 2025, anticipation builds over its outcomes and potential to revolutionize child obesity treatment.
Success could mean a new, effective tool in the fight against obesity, while failure or significant adverse effects could temper enthusiasm for pharmacological interventions. Either way, the trial’s findings will undoubtedly influence future approaches to treating childhood obesity.
A Balancing Act

The debate surrounding semaglutide’s use in children highlights a delicate balance between innovation in medical treatments and the ethical considerations of such interventions.
As society navigates these complexities, the ultimate goal remains clear: to find effective, safe, and sustainable solutions to combat childhood obesity.
The Road to Approval
As the trial progresses, it serves as science-based hope for those seeking new avenues to address child obesity. The journey toward broad acceptance and use of semaglutide for children is full of challenges, including proving its efficacy and ensuring its safety.
The outcome of this trial may well dictate the future of obesity treatment, offering hope to many while highlighting the ongoing need for comprehensive, balanced approaches to health and wellness.








































