Deep brain stimulation (DBS) has emerged as a potential treatment for severe depression, offering hope to those unaided by conventional therapies.
Emily Hollenbeck, a patient with a profound history of depression, underwent this innovative procedure. Researchers, like those at Mount Sinai West, are optimistic that DBS could significantly benefit nearly 3 million Americans who suffer from treatment-resistant depression, as it has already been approved for other conditions like Parkinson’s disease and epilepsy.
Emily Hollenbeck’s Personal Story: A Fight Against Depression

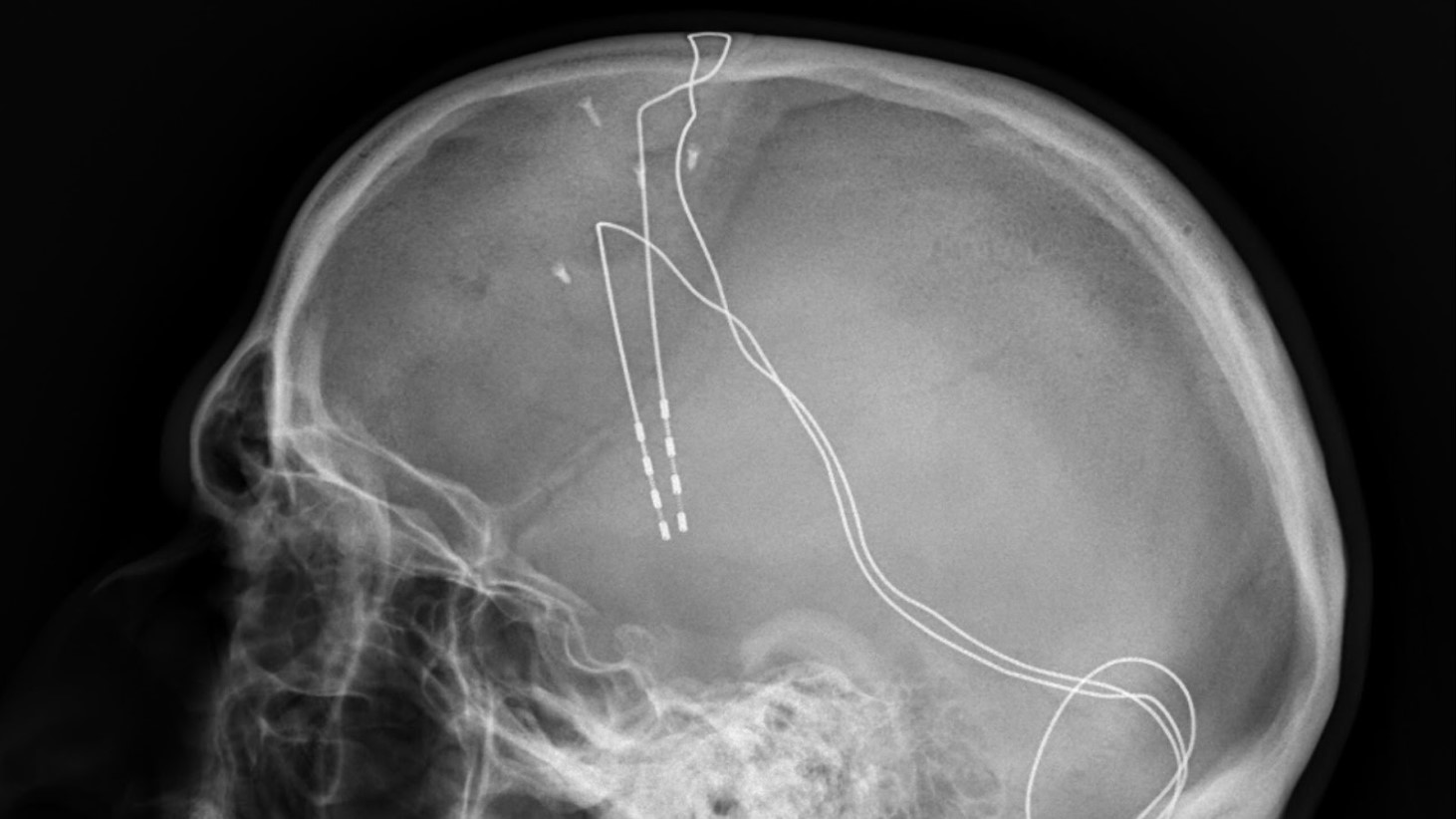
AP News reports that Emily Hollenbeck’s battle with depression was intense, with her describing it as being trapped in a black hole. Desperation led her to participate in an experimental DBS therapy, involving electrodes implanted in her brain.
This treatment, she hoped, would offer a respite from her relentless condition, having witnessed the dire consequences of depression in her own family, with both parents succumbing to it.
Interacting with the Brain’s Circuitry
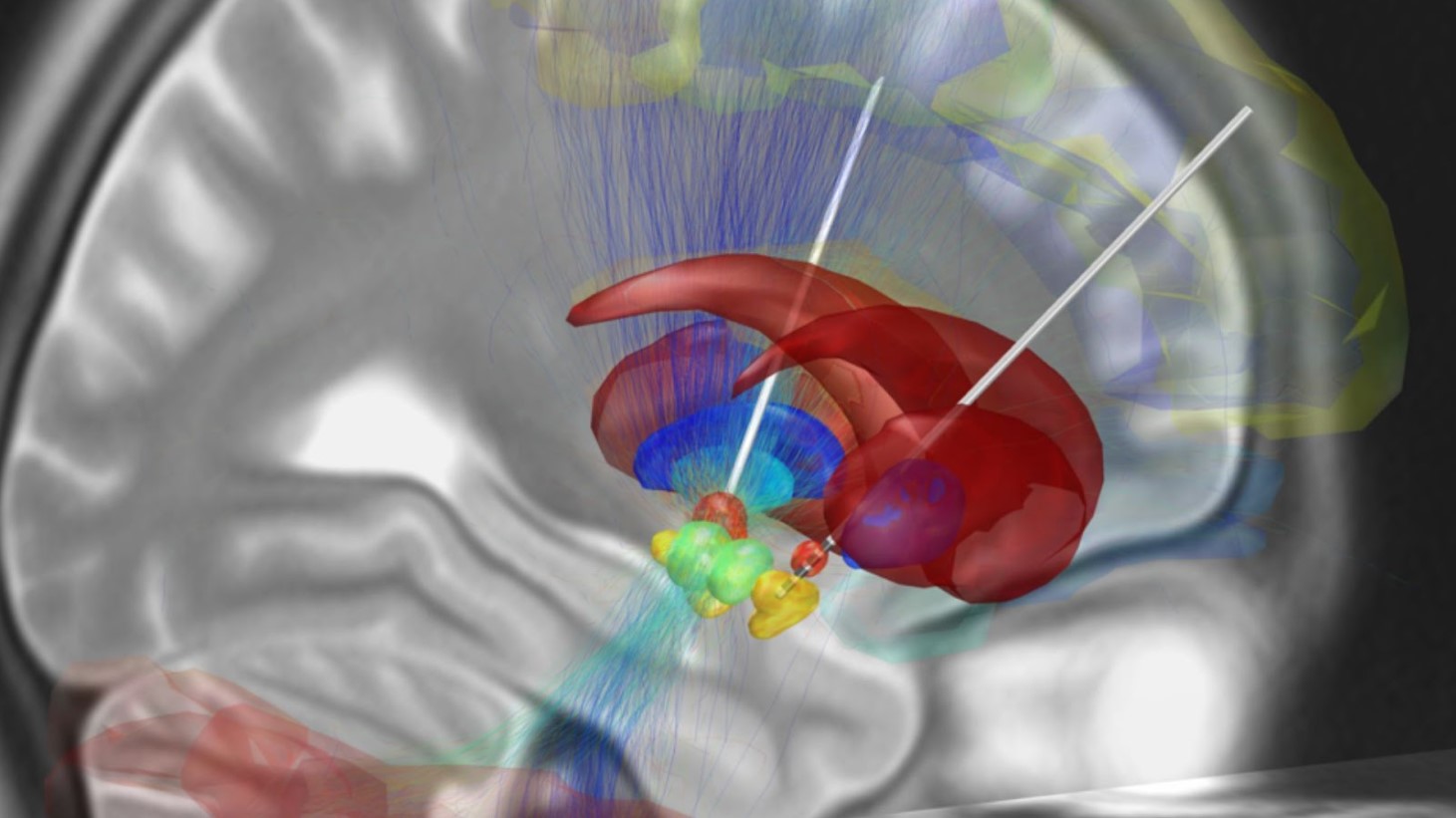
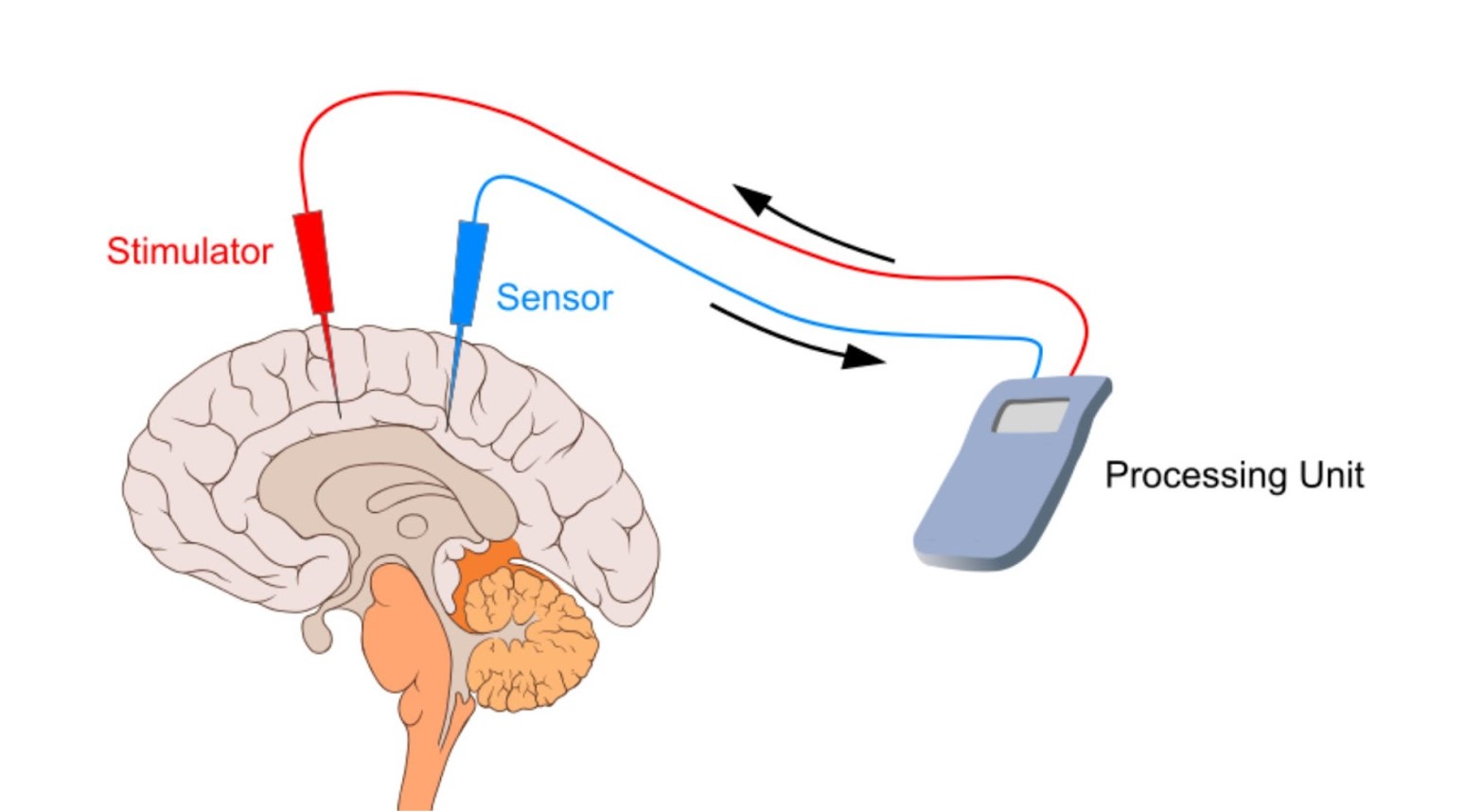
Johns Hopkins Medicine explains that DBS treatment functions by delivering targeted electrical impulses to specific brain areas, akin to a pacemaker for the brain.
Dr. Brian Kopell, involved in Hollenbeck’s treatment, explains that DBS helps to correct the abnormal electrical activity in depressed patients’ brains, facilitating a return to normal function.
Unraveling How Deep Brain Stimulation Works

DBS targets the disorganized electrical signals in the brain responsible for movement-related symptoms in Parkinson’s disease and other neurological disorders.
By implanting leads in the brain, connected to a neurostimulator under the collarbone, DBS delivers continuous electric pulses to interrupt these irregular signals.
The Precision Behind DBS Implementation
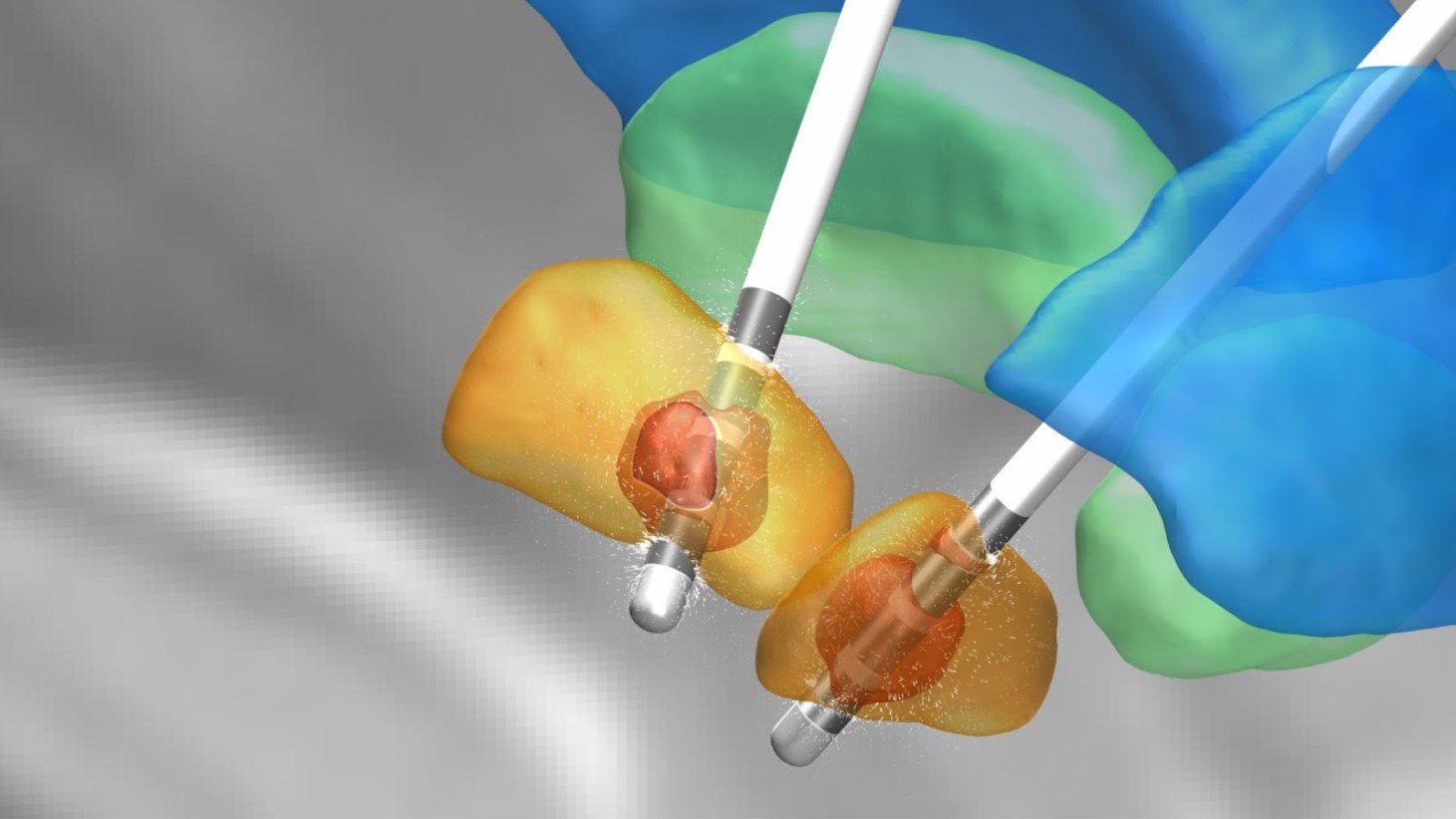
Following careful testing to ascertain the best lead placement, neurosurgeons implant the system, initiating a series of programming sessions post-surgery.
These sessions are crucial to fine-tune the neurostimulator’s electrical output, aiming for the sweet spot where symptom relief is maximized, and side effects are minimized. This meticulous adjustment process is key to the success of DBS therapy.
Research and Approval: Expanding DBS to Depression

The FDA is accelerating its review process for Abbott Laboratories’ request to use DBS devices for treatment-resistant depression, signaling a promising step toward broader application.
This comes as a beacon of hope for many, reflecting a growing body of research supporting DBS’s effectiveness.
Overcoming Adversity: Emily’s Journey to Recovery

After the DBS procedure, Hollenbeck began to experience significant relief from her depressive symptoms.
She recounted feeling an immediate lightening of her mood, an effect so profound that she could savor the taste of food and enjoy music once again, activities that her depression had stripped of pleasure.
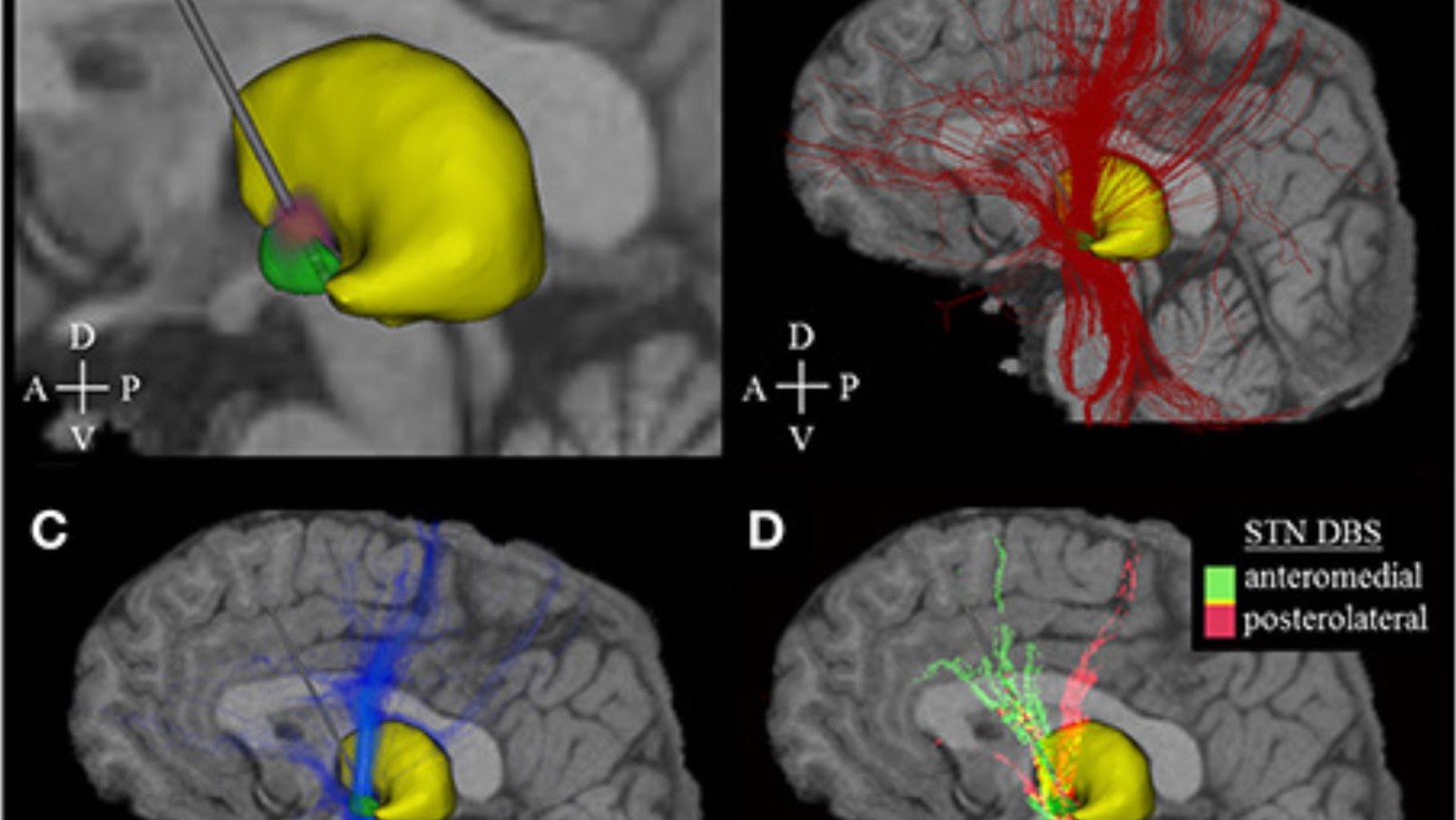
Personalization in Treatment: Tailoring DBS to the Patient
The New York Times details that the approach to DBS in depression treatment is increasingly personalized, taking into account the unique brain patterns of each patient.
This individualized method aims to enhance the effectiveness of DBS, ensuring that the electrical stimulation is optimally targeted. Mount Sinai’s research team, among others, is at the forefront of this innovative practice.
Real-life Impact: Patients’ Experiences with DBS

Patients who have undergone DBS for depression report significant improvements in their quality of life.
These personal accounts underscore the potential of DBS to provide relief for those who have exhausted other treatment options. While not a miracle cure, DBS represents a crucial step forward in the management of severe depression.
Challenges and Concerns: A Balanced View of DBS
Despite the promising results, skepticism remains regarding DBS for depression.
Critics, like Dr. Stanley Caroff, an emeritus professor of psychiatry at the University of Pennsylvania, emphasize the need for a deeper understanding of depression’s neural mechanisms before DBS can be universally adopted. The scientific and medical communities continue to explore these questions, balancing optimism with a rigorous scrutiny of the evidence.
The Continuing Care Post-DBS

Following DBS, patients like Emily Hollenbeck continue to require care and monitoring.
AP News explains that the treatment is part of a comprehensive management plan that includes ongoing medication and therapy.
The Journey Ahead: Optimism and Realism in DBS Research
The path forward for DBS in depression treatment is marked by cautious optimism. AP News notes that as researchers like Dr. Helen Mayberg and Dr. Katherine Scangos continue to explore DBS’s mechanisms and applications, the medical community remains hopeful yet vigilant, ensuring that advances in DBS are grounded in solid scientific evidence and ethical practice.
The ultimate goal is to enhance the lives of those battling severe depression, offering them a new avenue for hope and recovery.








































