As summer gatherings commence, Americans are once again experiencing a rise in COVID-19 cases.
Predictably, case numbers increased during the winter when more people were indoors. Now, as anticipated by experts, cases are climbing with the onset of summer.
Covid’s Persistence
Data from the Centers for Disease Control and Prevention (CDC) shows small increases in hospitalizations, deaths, and new cases.
This recent rise underscores the virus’s persistence, four years into the pandemic.
An Endemic

“When you begin to see a pattern, you then might say it’s becoming endemic,” Dr. Jessica Justman, a professor of epidemiology and medicine at Columbia University, told USA TODAY.
“When something is endemic, that does not mean it’s going away. That means it’s staying around.”
Still Affecting the World

Americans have similarly adapted to preventing seasonal flu, another endemic disease.
Like any virus, SARS-CoV-2 continuously mutates to infect more people and survive.
Taking Pro-Active Measures

These new variants and sub-variants, akin to tree branches, each feature unique mutations aimed at adaptation.
Health experts and officials have responded to these changes with vaccines and other measures to mitigate the risk of severe illness and overburdened health systems.
Lower Figures of Covid-Related Deaths

The recent upticks in sub-variants are significantly lower than the levels seen in 2020 or during the omicron surge in 2021.
Hospitalizations and emergency room visits are much less frequent than they were in December, and deaths have not reached the winter peak of over 2,000 weekly deaths in January. As of June 15, the latest CDC estimates indicate fewer than 150 COVID-19-related deaths.
Sub-Variant FLiRT

Current cases are primarily driven by consistent upticks in a group of sub-variants known as FLiRT, named for their technical mutations.
FLiRT originates from the JN.1 variant, which had dominated cases until the spring.
Most Prevalent in the U.S.
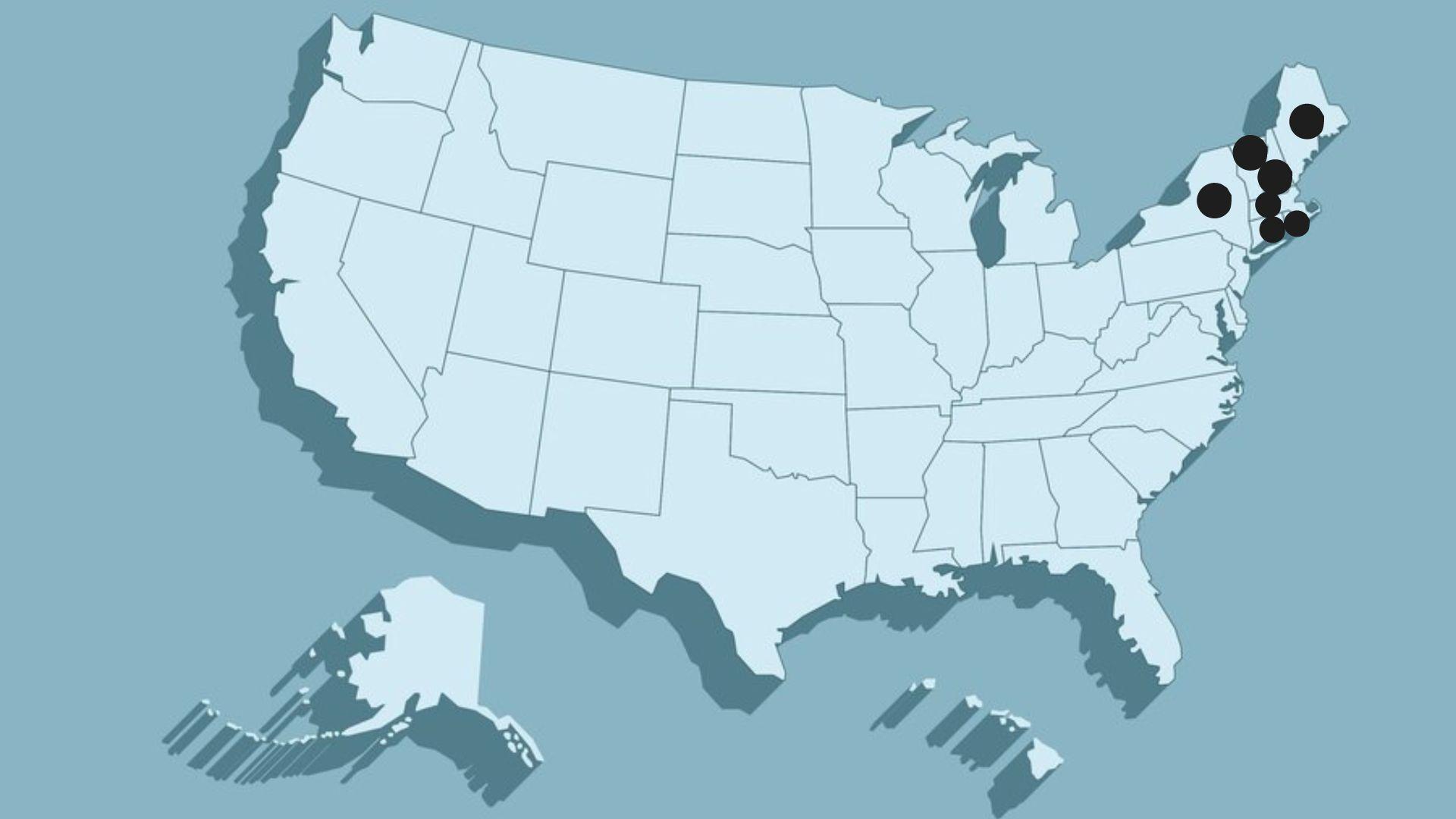
Now, FLiRT is increasingly prevalent in the U.S., with the KP.3 sub-variant accounting for about a third of cases, followed by KP.2 and KP.1.1, according to CDC data.
The LB.1 variant, also derived from JN.1, is another significant contributor to the circulating variants.
Difficult to Accurately Measure
The western U.S. and Hawaii have reported recent increases, as CDC data indicates. However, wastewater samples across the U.S. also suggest a broader increase in the virus’s spread.
Michael Osterholm, director of the University of Minnesota’s Center for Infectious Disease Research and Policy, acknowledged that some new cases involve the FLiRT variant but noted the U.S. lacks robust surveillance at this stage of the pandemic. “It’s fair to say that there is an increase,” he said. “What we don’t know yet is how much it’s going to be.”
More Transmissible

FLiRT may be more transmissible due to mutations that help it evade antibodies, according to Andy Pekosz, a professor of molecular biology and immunology at Johns Hopkins Bloomberg School of Public Health.
However, it does not appear to cause more severe illness or present different symptoms.
Importance of Vaccines
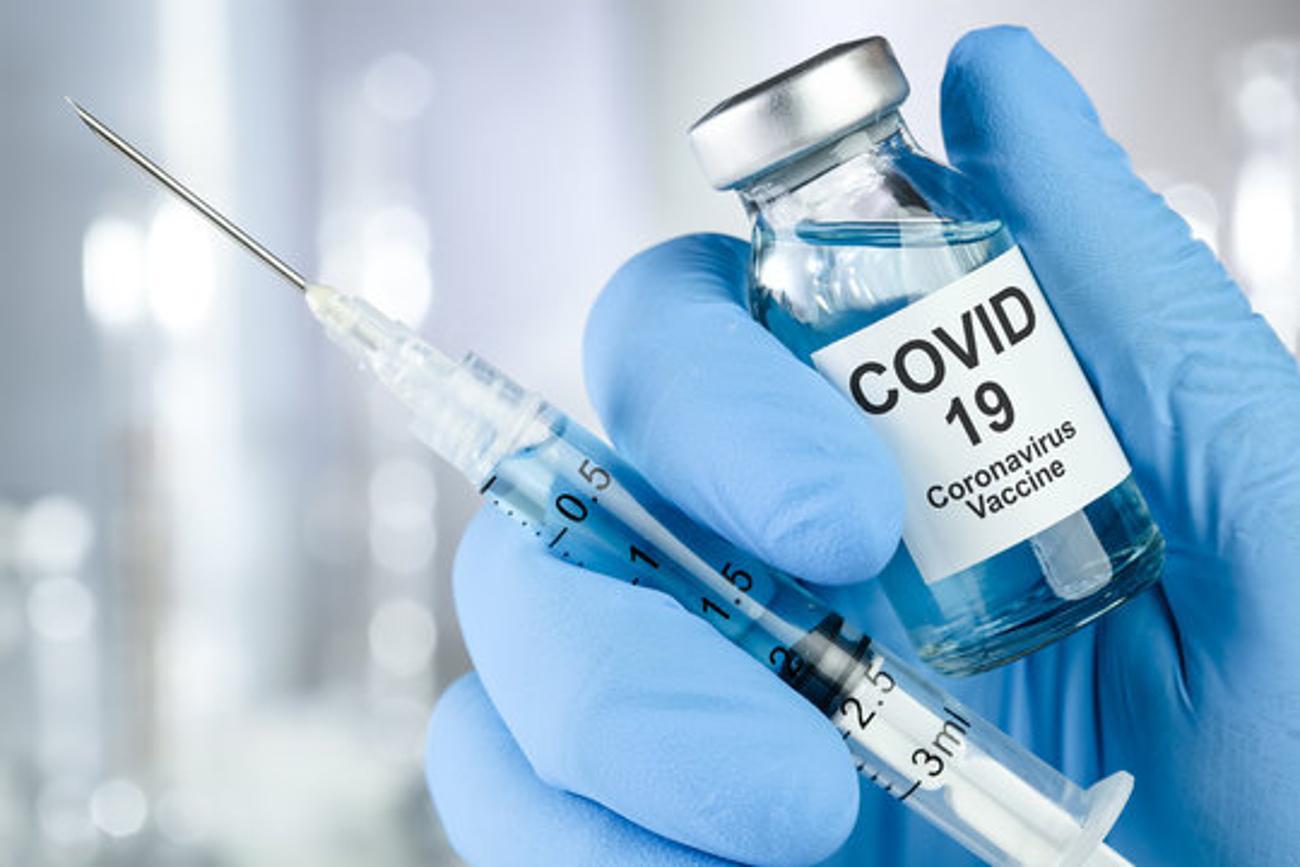
Vaccines continue to offer protection against COVID-19, although their effectiveness may diminish over time.
The last vaccine, introduced in late 2023, targeted the XBB.1.5 variant. In February, the CDC advised people 65 and older to get a booster of the current vaccine.
Continuous Development of Vaccines

In early June, a Food and Drug Administration advisory panel recommended that vaccine manufacturers target the JN.1 lineage. A new round of vaccines is anticipated in late summer or early fall.
To reduce the virus’s spread, individuals with respiratory symptoms should stay home and contact healthcare providers for treatment if at serious risk of illness. Experts continue to recommend wearing masks and practicing social distancing to minimize COVID-19 transmission.








































